These specialists focus on educating and offering alternatives to patients in the later years of their lives.
| 2019 Q4 | story by Liz Weslander | photos by Steven Hertzog

OB-GYNs are most commonly associated with delivering babies and caring for women in their childbearing years. But once those babies grow up, and the reproductive years come to an end, a woman’s pelvis still needs love. While incontinence, pelvic prolapse, vaginal atrophy and other physical and emotional challenges that tend to show up around menopause are not nearly as fun to talk about as pregnancy and babies, they should not be ignored.
Dr. Cathy Dahl and Dr. Samantha Durland are two local physicians who started out as OB-GYNs but have since followed unique paths to create distinct practices that focus on optimizing the health and comfort of women in mid-life and beyond. These doctors are improving the lives of women through innovative and integrative approaches.
Addressing the Symptoms
Pelvic Health Specialists, is the practice of Dahl, who in 2013, became the first board-certified urogynecologist in the state of Kansas. Urogynecology is a subspecialty of obstetrics and gynecology that focuses on pelvic-floor disorders and requires additional training in female pelvic medicine and reconstructive surgery. She is currently the only board-certified urogynecologist in the Lawrence and Topeka area.
Dahl says her practice most commonly treats urinary incontinence, fecal incontinence, pelvic prolapse and pelvic pain through a variety of surgical and nonsurgical procedures. Because the symptoms for these conditions can overlap, Dahl says patient visits at her practice last 45 minutes to an hour to allow plenty of time to thoroughly address symptoms.
“There are lot of things we do in this specialty, and we offer lots of surgical and nonsurgical options,” Dahl explains. “We make sure we address the symptoms patients are having and assess what they are really related to. We make sure that patients go home with answers to the question they came with.”
While surgery is sometimes the best option for Dahl’s patients, she also offers a number of innovative, minimally invasive procedures and will always try to match patients with those treatments when appropriate.
In 2020, Pelvic Health Specialists will add pelvic-floor physical therapist Sarah White-Hamilton, DPT, to the practice. Pelvic-floor physical therapy can help with surgical recovery but is often a viable, nonsurgical option for patients dealing with pelvic issues.

L: Dr Durland sitting on the front desk at Simple Wellness; R: Samantha White-Hamilton, pelvic-floor physical therapist at Pelvic Health Specialists.
“If someone is coming to me, and they are having urinary leaks and don’t want to have surgery, then a lot of times my urinary incontinence patients don’t have to have surgery,” White-Hamilton explains. “There are also some degrees of pelvic prolapse where we can stabilize things and make people more comfortable with strengthening and coordination. That’s what I like about working with Dr. Dahl, is that she gives them all the options.”
White-Hamilton says the role of a pelvic-floor physical therapist is to help patients gain coordination in their pelvic-floor muscles, which starts with helping patients understand exactly where the pelvic-floor muscles are located.
“A lot of the time, I say ‘pelvic floor,’ and people give me a blank stare because, in our society, there is not a lot of education around that. It’s getting better, but we don’t know our bodies all that well,” Hamilton says. “I hear so many women who say they have been dealing with their symptoms for 20 years and didn’t think there was anything they could do about it. I just want to scream from the rooftops with a bullhorn that there is hope, and there is help.”
Once a patient has a proper awareness of the location of the pelvic-floor muscles, she can start to address specific issues. White-Hamilton says common symptoms she addresses are leaking when laughing, coughing or sneezing, or needing to constantly run to the bathroom. While strengthening the pelvic floor is usually part of the picture, symptoms such as pain with intercourse, difficulty emptying the bladder and constipation are often the result of tight pelvic-floor muscles, which means working with patients to relax the muscles, she continues.
“One of the biggest misconceptions about pelvic-floor physical therapy is that it’s all about the Kegels; but if your muscles are tight, and you cannot relax, there it absolutely no point in trying to strengthen it,” White-Hamilton explains.
In addition to physical therapy for the pelvic floor, Dahl’s practice also offers bladder Botox treatment for urinary incontinence, where Botox is injected into the muscle of the bladder in order to decrease muscular contractions. While this procedure has been available for 20 years, the FDA did not approve Botox for overactive bladder until 2013. The FDA approval means that insurance will now cover in-office bladder Botox treatments, which is convenient for the patient.
Neuromodulation, which works through an implantable device that regulates sacral nerves to relieve both urinary and fecal incontinence, is another minimally invasive and innovative treatment Dahl offers.
“It’s kind of like a pacemaker would be for the heart, but it’s for pelvic nerves,” Dahl explains. “It is one of my favorite things we do here, because it changes people’s lives.”
She says her practice manages its own neuromodulation devices, which is not typical but provides both convenience and better patient outcome.
“We test the device here to see if it helps patients, and if it does, we take one visit to the operating room to implant the hardware,” Dahl explains. “Most physicians don’t program and manage the devices afterwards, but we do, and we are able to make sure patients really get the best outcome.”
Vaginal rejuvenation laser treatment for vaginal atrophy is another innovative procedure Dahl’s practice offers. Vaginal atrophy is caused by a drop in hormone levels, which often occurs during menopause or after childbirth, she explains. The drop in hormones causes the vaginal area to get dry and the tissue to thin, which can cause pain during sexual activity, general irritation and infection. Vaginal rejuvenation laser therapy stimulates the production of healthy vaginal tissue and is a good alternative for those who cannot, or prefer not to, do estrogen-replacement therapy, the more traditional treatment for vaginal atrophy. The primary downside of the vaginal rejuvenation procedure is that it is not covered by insurance, so patients have to pay out of pocket, Dahl says.
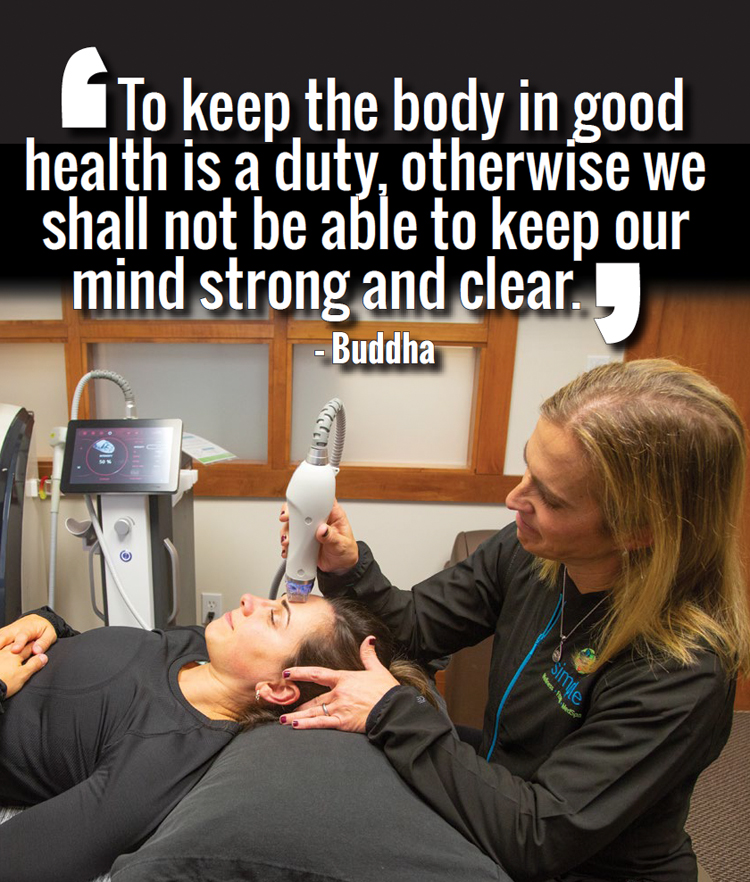
Dr. Samantha Durland performs a skin rejuvenation procedure with the Secret RF – a microneedling device that uses radio frequency to deliver an individual-ized treatment for fine lines, wrinkles, acne scars, and photo damage.
Navigating the System
While treatments that are not covered by insurance have some obvious downsides, Dr. Samantha Durland, MD, another local OB-GYN who works with the middle-aged population, has found working outside of insurance can mean more options for patients.
Durland has been a practicing OB-GYN for two decades, but in 2015, she completed a fellowship in Metabolic and Nutritional Medicine, and then became board-certified in antiaging and regenerative medicine. Durland has since shifted the focus of her practice from traditional OB-GYN to an integrative model that treats both women and men, and operates outside of insurance.
“I tend to help people with noninvasive procedures by combining holistic and classic westernized approaches,” Durland explains. “That’s something I couldn’t really do in traditional medicine. I have moved to where I am right now in a journey to help people get better in a way that makes more sense to me.”
Durland’s practice, Simple Wellness, 4811 Bob Billings Pkwy., offers a broad spectrum of wellness and antiaging services. She says rising deductibles and lack of transparency of costs contributed to her decision not to work with insurance networks. Not being contractually obligated to the insurance companies allows her to navigate the system more cost-effectively and offer patients more choices.
“Lawrence is a very educated community, and there are a lot of people seeking alternatives,” Durland says. “One size does not fit all, and I need to have all the options open. At this point in time, I am not restricted in my ability to have conversations with patients about what options are out there. That lack of restriction hopefully allows me to do a better job.”
Middle-aged women make up a large portion of Durland’s patients, and Durland says getting women comfortable with talking about the issues they face is an important aspect of her practice.
“The post-childbearing years are when women start to feel tired all the time, and things like stress urinary incontinence or sexual function start to come up,” Durland explains. “People are afraid to talk about it and don’t even know how to start the dialogue – and can end up feeling very alone. You are not alone; you are normal, and it happens to all of us. So much of what I love to do is listen and try to demystify a lot of emotion that we have with conversations about things happening to our body.”
One nontraditional treatment Simple Wellness offers for menopausal women is bioidentical hormone-replacement therapy, which uses natural hormones to replace those lost in the aging process.
“In classic westernized medicine, hormone-replacement therapy is usually pharmaceuticals,” Durland says. “Bioidentical hormone-replacement therapy is making sure that the chemical structure that you are returning to the body are the same chemicals that the body produces. It also includes testosterone for women, which is not typically considered in traditional western medicine.”
Durland offers vaginal rejuvenation laser therapy similar to treatment offered by Dahl but also performs platelet-rich plasma (PRP) therapy for vaginal rejuvenation.
“It’s a process where we take your blood and spin down your healing factors, and then inject that back into the area that we would like to heal,” Durland says. “It is a complement to a lot of procedures, because the human body is the best at healing itself.”
PRP can also be used to treat erectile dysfunction, and, as an added bonus, the procedure also is one of the only nonsurgical male enhancement treatments that can increase penis size.
“I think the statistic is that 80 percent of the family medical decisions are made by a female,” Durland says. “So a lot of males that we see have been sent by significant others. But once you get them in here, and they start talking, it’s really about education and understanding alternatives and options, and not feeling alone.”