Though genetics play a major role in whether you will develop heart disease, don’t forget about the importance diet and exercise.
| 2019 Q4 | story by Bob Luder | photos by Steven Hertzog
In this internet age of Google and YouTube, information and advice about anything, including good heart health and wellness, is readily available at the touch of your fingertips. Walking regularly, eating a lot of fresh fruit and vegetables, and staying away from smoking and alcohol are just a few of what are an endless array of tips, opinions and programs that promote and encourage healthy tickers.
But according to at least one heart expert, it’s probably wise to treat much of what is on the internet about heart and heart health with a sharp degree of skepticism. Opinions are a dime a dozen. Facts are all that matter.
“Expert opinion is worthless,” says Dr. Roger Dreiling, MD, interventional cardiologist at Lawrence Memorial Hospital. “Show me the data.”
That data, he says, points to a couple of key factors when it comes to heart health and whether one might be at risk of developing heart disease now or in the future. The most important has to do with who gave birth to you. Genetics play a major role in coronary artery disease, especially with two forms of disease known as dilated cardiomyopathy and familial atrial fibrillation.
“If you know the heart histories of your great-grandparents and grandparents,” Dreiling says, “you have a good idea of how long you’ll live.”
Hypertension, abnormally high blood pressure and especially arterial blood pressure, is a major cause of heart disease and can be genetic or dietary, explains Dreiling, who estimates he’s performed some 10,000 catheterization procedures in his 30-plus years of practice. If parents, grandparents or even great-grandparents lived with hypertension, it’s quite possible it was passed down through generations. Hypertension also can be prompted by a diet that includes a high amount of sodium.
“If you can pull it out of a freezer or icebox, or take it out of sealed packaging, don’t eat it,” Dreiling says. “Things like processed meats contain a lot of sodium.”
He advises simply not buying salt when visiting the grocery store.
“If you don’t have salt in the house, you can’t eat it,” he says. “If you cook your own food and don’t have salt in it, you’re eating a heart-healthy diet.”
And that gets to the second major factor that contributes to heart disease: being overweight. It’s vital to maintain a suitable body weight. Have your BMI—body mass index, which is weight indexed to height—checked and take steps to get within the medically recommended range.
“Thirty percent of the people I see have a BMI (body mass index) of 25 or less,” says Dreiling, referring to those within the range of a healthy weight/BMI. “Obesity is an epidemic in this country, and that contributes to hypertension and sleep apnea.”
Lastly, exercise. Daily exercise of at least 20 minutes can go a long way toward maintaining good heart health.
“These are the things we have control over,” Dreiling says. “Everything in moderation.”
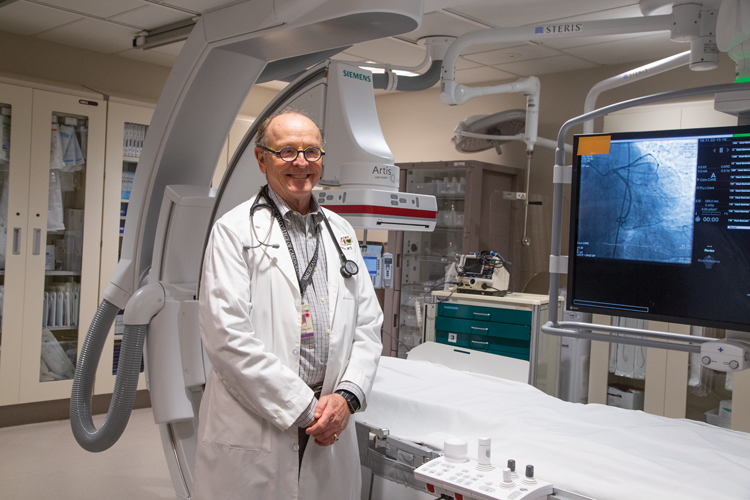
Dr. Roger Dreiling, MD, interventional cardiologist in the new state of the art cardiology unit at LMH.
Men vs. Women
Once upon a time, it generally was believed that heart disease was a plight specified to men only. Women didn’t have to concern themselves about it.
That was because in the past, women were largely ignored when it came to the study of heart health and heart disease.
“Historically, women were not well-represented in cardiac trials,” says Dr. Christina Salazar, MD, a cardiologist at Lawrence Memorial Hospital. “In all major trials; women’s representation was low.”
In more recent times, the opposite has been proven true. Studies have shown that cardio disease is the No. 1 killer of women in the U.S. And many of the risk factors for women with heart disease are the same as for men. Some, however, like obesity and diabetes, affect women more.
Unfortunately, the news doesn’t get much better for women.
“Women tend to do worse (than men) when they are diagnosed,” Salazar says. “And while cardiac disease has been on the decline in recent years, it hasn’t been as much in women.”
The reason for that, she continues, is the same reason women’s health, in general, often suffers more than males: They simply don’t take the time to take care of themselves. That could explain why women tend to deal with blocked arterial disease more in their 70s as opposed to 60s for men.
“Women tend to not receive as much therapy,” Salazar says. “They tend to focus on other things than themselves.”
There are other differences in heart issues among those of the opposite gender. Dreiling and Salazar agree men tend to present symptoms of heart problems, on average, about 10 years earlier than women. When men do present, it’s usually in the form of a heart attack. When women present, it’s typically angina, or chest pain caused by an inadequate supply of oxygen to the heart muscle. Angina can accompany or be a precursor of a heart attack.
Angina can be brought on by high stress levels, Dreiling says. But he dismisses anxiety and stress as real contributors to heart disease, while admitting there is something known as “broken heart syndrome,” an extreme grief reaction in which the science is not completely understood.
“I don’t think (someone under stress is) any more or less prone to developing disease,” he says. “Most (who are prone to disease) are liable to be smokers, overweight or drug users.”
There also could be hormonal factors in play when women reach menopause, but more study is needed in that area, Salazar explains.
Also, blockages in women tend to be in the smaller capillaries compared to men, whose blockages typically occur in the larger, major arteries and veins. Salazar suggests thinking of it in terms of tree limbs growing smaller the farther they grow from the trunk.
“Women’s heart disease is usually more microvascular, or the little limbs on trees,” she says. “In most of those instances, the only treatment is medical therapy.”
“The data has shown that microvessel disease may be more due to gender, smoking and diabetes,” Dreiling says.
Despite the increasing awareness of women’s heart health, Dreiling says that most of his experience in treating heart disease involves men.
“For every five catheterizations I do, the ratio is four men to one woman,” he states.
The good news for women, Salazar says, is that increasing communication avenues such as social media are helping raise more awareness for women and heart-health issues, bringing about more national panel discussions on related topics.

Dr. Christina Salazar, MD, cardiologist talks to her patient using a heart model.
Strokes and Treatment
Hypertension, along with high cholesterol levels, are contributors to a condition formally known as carotid atherosclerosis. It is more commonly referred to as a stroke.
Strokes are the No. 5 cause of death and a leading cause of long-term disability, claiming the lives of more than 134,000 people annually. They are caused when one develops plaque—fatty, waxy substances that form deposits on arterial walls—that reduce blood flow. When one experiences a rupture of one of these plaque deposits, a stroke occurs.
Dreiling says there also are embolic strokes, which is an instance of a blood clot in the heart that travels to the brain. It occurs when there is atrial fibrillation (an irregular, rapid heart rate) and is a more common form of stroke. It also can be a more dangerous form of stroke in that it often can go unrecognized.
There are, however, visible signs of carotid atherosclerotic strokes, which is important because the sooner a stroke can be treated, the better chance of survival and recovery. A common acronym to remember for stroke awareness is F.A.S.T. to help recognize symptoms and know what to do.
- F: Face weakness
A: Arm weakness
S: Speech difficulties
T: Time to call 9-1-1
If caught early enough, aspirin can be a stop-gap treatment for atherosclerotic carotid disease. However, Dreiling warns that aspirin is rarely suitable for patients experiencing atrial fibrillation.
In most cases, stroke is not inevitable. Knowing the health risks and managing blood pressure and diabetes through good nutrition and exercise habits are the keys to avoiding one of life’s most common heart disease-related maladies.
Tests for Heart Health
There are a number of at-home self-checks people suspicious of heart issues can perform to assess their risk. Do you have symptoms? Is there chest discomfort, shortness of breath or ankle swelling? How long have symptoms been present? When were they first noticed? Finally, again, checking family history is important.
There also are a number of formal testing procedures folks can undergo at their doctors’ offices or a hospital that can go a long way toward assessing heart health.
The foremost test used is the electrocardiogram, more commonly referred to as an EKG, in which electrodes are secured to the patient’s chest, and an electronic readout of heart activity is recorded. From that readout, a cardiologist can determine whether one has experienced a heart attack or is having one.
A stress test, of which there are several iterations, basically involves hooking patients up to an EKG and placing them on a treadmill to record how the heart reacts to being put under stress through physical work.
“We’ve found some instances where women have false-positive tests,” Dreiling says. “(To get an accurate test), it needs to be someone who can walk and has a normal (sitting) EKG.”
He explains there also are treadmill EKGs where the patient is injected with a radioactive substance, and photographs are taken of heart activity to determine where blockages exist. In addition, there are chemical stress tests that dilate the arteries to check for blockages.
“A normal stress test means that medicine will do everything I can do for you,” Dreiling adds.
Cardiologists today also can perform computed tomography (CT) scans looking specifically at coronary activity. These scans are called CTA, or computed tomographic angiography.
There’s a CT scan that looks specifically for calcium, one of the major culprits in plaque buildup and blockages. It calculates a coronary calcium score, which detects the quantity of plaque in the arteries, and often is used on patients reluctant to ingest a pill or undergo a traditional stress test.
The means to determine heart health and disease risk are vast, whether by at-home self-assessment or formally by a medical provider. What’s important is to not judge solely on the opinions of others or strictly follow the advice of friends. Check the facts. Stay in tune with how you feel. And stay well-educated on your family’s heart-health history.
As Dreiling says, “Show me the data.”
“There’s an age where you don’t have to worry about heart health, and that’s 95,” he says. “If you’re born in the U.S. and are eating a western diet, then you should always be cognizant of your health.”